Evaluating Risk
By Elisabetta Tola / 5 minute read
Many science stories — especially health stories — attempt to quantify risk. Often, it is done as a ratio or percentage, as in the American Heart Association’s estimated risk of an adult in the United States contracting a cardiovascular disease in his or her lifetime: 48 percent. Huge, right?
First, one must understand what cardiovascular disease is. It includes not just coronary heart disease, heart failure and stroke, but also high blood pressure. Remove that last category, and the risk drops to 9 percent.
Absolute Risk
That 9-percent figure is an estimate of the absolute risk, or the percentage of people in the entire U.S. population who are likely to contract the disease. It pays no attention to individual risk factors like genetics, smoking, or regular exercise, unless the population itself is limited by those factors. (In other words, if the entire population being studied is made up of smokers, then the absolute risk is for people engaging in that behavior.)
Of course, the reality is that everyone has a different risk, depending on various factors. Some are independent of an individual’s behavior. Age, family history, and gender are out of a person’s control. Other factors more likely to be under a person’s control include nutrition, exercise, smoking, and drinking. There are also conditional probabilities to consider: one’s risk of a heart attack might be higher if one previously suffered a heart attack.
Relative Risk
That’s where relative risk and odds ratio come in. Both figures are ratios, but they are two different measures applying to different type of studies. Researchers calculate relative risk when doing a prospective study; i.e., a “cohort study,” in which people are observed and data are collected following them in real time. An odds ratios is calculated in a retrospective study, also called a “case-control study,” in which researchers compare two selected samples of people — for example, a group of people with HIV and a group without it.
Relative risk (sometimes abbreviated to “RR” and also called risk ratio) is calculated by dividing the risk of the population exposed to a certain factor (smoking; unhealthy diet; sedentary lifestyle) by the risk of the unexposed population. For each cohort, researchers will measure the incidence of the disease by calculating the ratio of affected people to the total number of people in that cohort. Finally they divide the incidence in the exposed population (for instance, smokers) with that of the unexposed population (nonsmokers).
As an example, let’s do some math using data from an article in the British Medical Journals’ Heart. According to the data, the lung-cancer mortality rate for smokers is 209 per 100,000 people; for nonsmokers, it is 14 per 100,000. Divide 209 by 14 and you get 15 (14.93, to be precise), which is the increase in the relative risk of dying from lung cancer if you smoke.
That “15” can be expressed in a variety of ways: 15 times, by a factor of 15, or a 15-fold increase. All mean the same thing. Alternatively, it can also be converted to a percentage increase. To do that, employ the “NOO” formula, which is outlined later in this chapter. Doing so would show you that smoking increases your risk of dying from lung cancer by 1,400%. However, such percentages are difficult for most people to understand, so we recommend sticking with the “15 times” phrasing, for clarity.
A relative risk below “1” means there is an inverse relationship between the factor and the outcome. For example, if the smoking group had fewer lung-cancer deaths, you would have a relative risk below 1, suggesting that smoking is a prophylactic against dying of lung cancer. You would expect to see figures below 1 for tests of effective drugs.
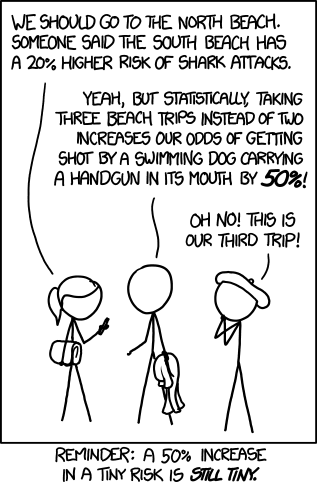
When reporting on relative risk, it is important to always mention the original absolute risk. If the original incidence of a disease is very low, reporting only on a large relative risk will lead to an overstatement of the effects of that risk factor. For example, if a study reports that in a group of 100,000 people just one person dies of lung cancer, while in the comparison group, two people out of 100,000 die, that is a doubling of relative risk, but the absolute risk is still quite small.
On the other hand, when the disease has a very high incidence, even a small difference in relative risk translates into high numbers of people who might be affected.
Odds Ratio
Sometimes a study will report an odds ratio instead of relative risk. This is common in a “case-control study,” in which researchers identify people with a disease or condition of interest and compare that group with another group that resembles the first but without the disease or condition. In such a study, the controls are not in place to determine relative risk. Instead, researchers can describe only probability or odds.
For example, imagine that researchers are looking at two groups of former lifeguards. One group contracted skin cancer, while the other group did not. By looking at the lifeguards’ use of the sunscreen zinc oxide, the researchers are able to calculate their odds of contracting skin cancer if they did or did not use zinc oxide. But, the researchers would not be able to calculate a generalized reduction in risk that using zinc oxide would provide to a random population.
To further explore this odds-ratio example, let’s pretend that the “case study” group of lifeguards who contracted skin cancer is made up of 100 people, of which 10 used zinc oxide. The “control” group consists of 400 lifeguards, of whom 300 used zinc oxide. To calculate the odds ratio that will tell you if the application of zinc oxide is protective against skin cancer, you would first look at the number of lifeguards who used zinc oxide versus those who didn’t in the case-study group of lifeguards who contracted cancer. Then divide the result by the ratio between those who used zinc oxide and those who didn’t in the control group.
The math, then, is your zinc-oxide users (10) divided by your non-zinc-oxide users in the case study’s cancer group (90) which is 0.11 (or 1 in 9). Next, divide the zinc-oxide users by the non-zinc-oxide users in the cancer-free group (300/100), to get 3. Finally, divide the first figure (0.11) by the second figure (3) to get 0.037, which is your odds ratio. You could say, “Lifeguards who use zinc oxide have 0.037 times the odds of getting skin cancer as lifeguards who do not use zinc oxide,” but that’s difficult to understand. Instead, divide the ratio into 1 and turn the sentence around to say more simply, “Lifeguards who do not use zinc oxide have 27 times the odds of getting skin cancer as lifeguards who do use zinc oxide.”
This is different from a risk assessment, since we don’t know the overall risk of getting skin cancer, nor were there controls for other factors. All we know is that, based on our made-up case study, the odds of getting skin cancer are 27 times higher for lifeguards who do not apply zinc oxide.
To summarize, when we calculate risk, we are looking at the number of cases within a population. But when calculating odds, we are comparing the cases with non-cases.